"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
31 year old male who is a photographer by occupation came to the casuality with complaints of Yellowish discolouration of sclera since 4 days ,Fever since 2 days which is insidious on onset , gradually progressive , subsided on medication. C/o Nausea and vomitings since 2 days Non -bilious and non projectile , food particle as content and was taken to local hospital in view of vomitings .
Patient was apparently asymptomatic 17 years back then his mom observed hypopigmented patch over the cheek , and multiple hypopigmentation patches areas all over the body , neglected thinking it was due to vitamin deficiency , 15 days back mother observed a hypopigmented patch on the right arm and took him to a local hospital and was diagnosed with hansens and was on treatment since then.
No complaints of shortness of breath, palpitations , headache , orthopnea, PND .
Non - Alcoholic
Non - Smoker
On examination
Patient is conscious coherent co operative
Oriented for time place and person
Pallor ++
Icterus ++
No cyanosis
Clubbing or lymphadenopathy
Febrile : 99.9
Bp: 130/80mmhg
PR: 83 bpm regular normal volume
CVS : s1s2 no murmurs
Rs : NVBS + no crepts
P/A: mild splenomegaly + BS +
CNS :
Tone : Rt Lt
UL N N
LL N N
Power : Rt Lt
UL 5/5 5/5
LL 5/5 5/5
Reflexes :
B S T A K P
Rt. 2+ 2+ 2+ 2+ 2+ F
Lt 2+ 2+ 2+ 2+ 2+ F
Sensory :
Fine touch : present
Crude touch : present
Lost sensation over the hypopigmented lesion on lower limbs
Intact sensation over the lesions on forearm & neck
(Touch , pain & temperature were intact over forearm & neck lesions
Lost pain & touch over lower limb lesions)
Diagnosis :
DRUG INDUCED HEPATITIS
BORDERLINE LEPROMATOUS LEPROSY
Treatment given:
1.TAB.UDILIV 300 MG/PO/BD
2.TAB.RIFAXIMINE 550 MG/PO/BD
3.SYP.LACTULOSE 10ML/PO/TID
4.INJ.PANTOP 40 MG/IV/OD
5.INJ.ZOFER 4MG/IV/SOS
6.IVF NS AND RL @50 ML WITH 1 AMP OF OPTINEURON IV/OD
7.MONITOR VITALS 2ND HRLY
DOA: 26/04/22
SOAP NOTES AMC DAY 1:
S
Yellowish discoloration of sclera since 4 days
Fever since 2 days
O
GENERAL EXAMINATION:
Patient is conscious,coherent, co operative
Oriented to time ,Place, Person
VITALS :
Temp 98.6 F
BP: 120/80mm hg
PR: 95bpm
RR: 17cpm
PER ABDOMEN EXAMINATION:
Mild Splenomegaly+
Bowel sounds present
CARDIOVASCULAR SYSTEM:
S1, S2 heard
RESPIRATORY SYSTEM:
BAE present, NVBS
CNS :NAD
Hb- 10.6
Urine bile salts and bile pigments positive
LDH 868 IU/L
Total bilirubin 7.82
Direct bilirubin 5.63
AST 401
ALT 580
ALP 208
A
DIAGNOSIS :
DRUG INDUCED HEPATITIS
?BORDERLINE LEPROMATOUS LEPROSY
P
1.TAB.UDILIV 300 MG/PO/BD
2.TAB.RIFAXIMINE 550 MG/PO/BD
3.SYP.LACTULOSE 10ML/PO/TID
4.INJ.PANTOP 40 MG/IV/OD
5.INJ.ZOFER 4MG/IV/SOS
6.IVF NS AND RL @50 ML WITH 1 AMP OF OPTINEURON IV/OD
7.MONITOR VITALS 2ND HRLY
SOAP NOTES AMC DAY 2:
S
Yellowish discoloration of sclera+
No fresh complaints
O
GENERAL EXAMINATION:
Patient is conscious,coherent, co operative
Oriented to time ,Place, Person
VITALS :
Temp 98.4 F
BP: 110/80mm hg
PR: 90bpm
RR: 18cpm
PER ABDOMEN EXAMINATION:
Mild Splenomegaly+
Bowel sounds present
CARDIOVASCULAR SYSTEM:
S1, S2 heard
RESPIRATORY SYSTEM:
BAE present, NVBS
CNS :NAD
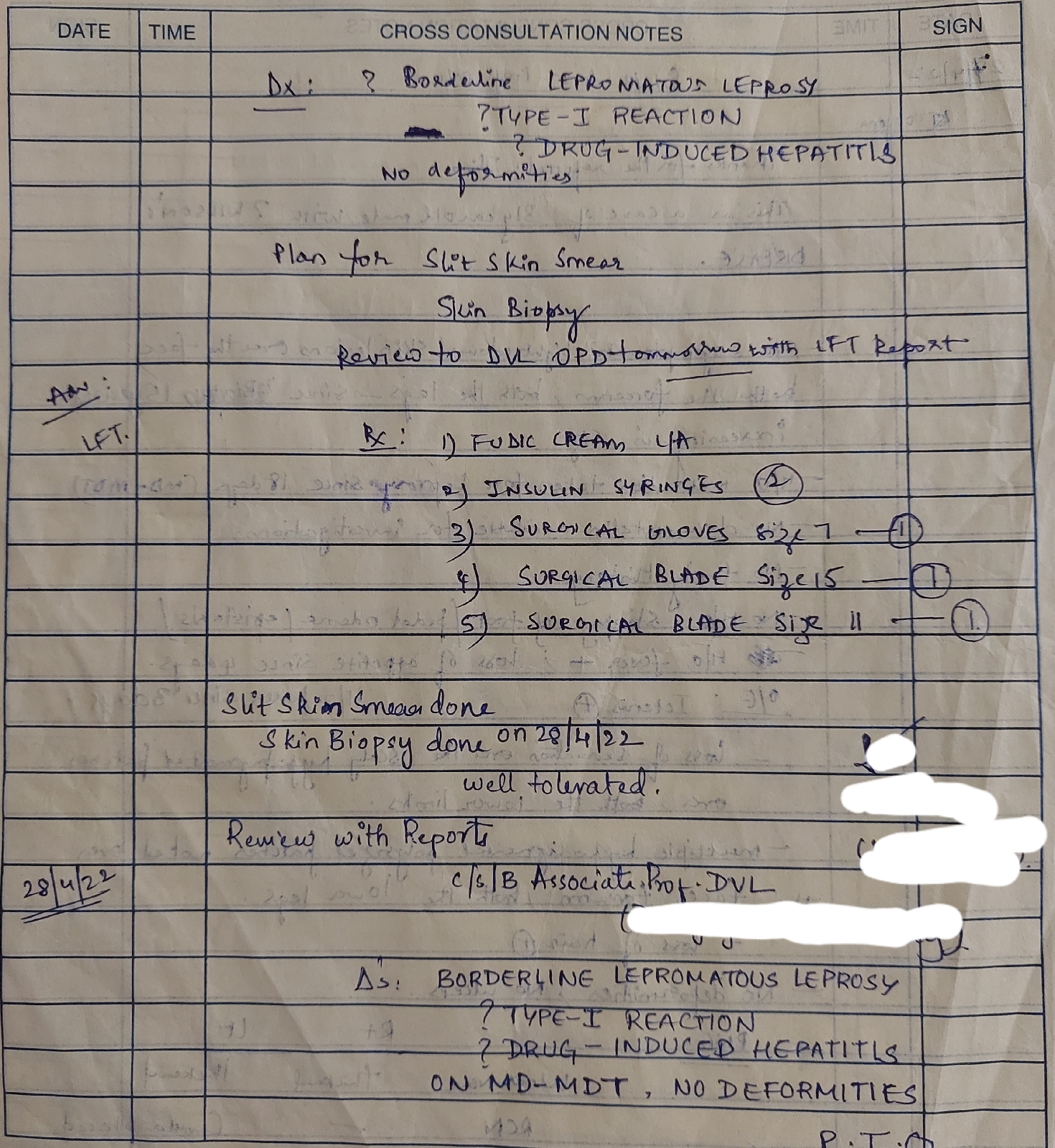
DVL referral: BORDERLINE LEPROMATOUS LEPROSY
Ophthal referral: B/L Heterochromia iridis
Direct Coombs test Negative
USG: No sonological abnormality detected
Today LFT(28/04/22)
MADDREYS DISCRIMINATORY SCORE: 21.3
A
DIAGNOSIS :
DRUG INDUCED HEPATITIS SECONDARY TO BORDERLINE LEPROMATOUS LEPROSY
P
1.NORMAL DIET
2.TAB.UDILIV 300 MG/PO/BD
3.SYP.LACTULOSE 10ML/PO/TID
4.INJ.PANTOP 40 MG/IV/OD
5.INJ.ZOFER 4MG/IV/SOS
6.IVF NS AND RL @50 ML WITH 1 AMP OF OPTINEURON IV/OD
7.SYP.HEPAMERZ 10 ML/PO/TID
8.FUDIC CREAM L/A
9.MONITOR VITALS 2ND HRLY
10.INJ.VIT K 1 AMP IN 100ML NS
SOAP NOTES AMC DAY 3:
S
Yellowish discoloration of sclera+
No fresh complaints
O
GENERAL EXAMINATION:
Patient is conscious,coherent, co operative
Oriented to time ,Place, Person
VITALS :
Temp 98.4 F
BP: 110/80mm hg
PR: 86bpm
RR: 16cpm
PER ABDOMEN EXAMINATION:
Mild Splenomegaly+
Bowel sounds present
CARDIOVASCULAR SYSTEM:
S1, S2 heard
RESPIRATORY SYSTEM:
BAE present, NVBS
CNS :NAD
On 29/04/2022:
Slit skin smear and skin biopsy done
MADDREYS DISCRIMINATORY SCORE: 21.3
A
DIAGNOSIS :
DRUG INDUCED HEPATITIS SECONDARY TO BORDERLINE LEPROMATOUS LEPROSY
DAPSONE SYNDROME
P
1.NORMAL DIET
2.TAB.UDILIV 300 MG/PO/BD
3.SYP.LACTULOSE 10ML/PO/TID
4.INJ.PANTOP 40 MG/IV/OD
5.INJ.ZOFER 4MG/IV/SOS
6.IVF NS AND RL @50 ML WITH 1 AMP OF OPTINEURON IV/OD
7.SYP.HEPAMERZ 10 ML/PO/TID
8.FUDIC CREAM L/A
9.MONITOR VITALS 2ND HRLY
10.INJ.VIT K 1 AMP IN 100ML NS
11.Tab.Omnacortil 20mg OD/PO after mrng breakfast.
12 .Tab.Omnacortil 5 mg OD/PO after dinner.
1/05/22
SOAP NOTES AMC BED -2
S -
Yellowish discoloration of sclera +
No fresh complaints
O- Patient is consious, co-herent, co-operative
No icterus,odema,cyanosis, clubbing, lymphadenopathy.
VITALS :
Temperature - 98.1F
Pulse rate - 84BPM, REGULAR, NORMAL VOLUME
BP -
@8AM-120/70MM OF HG
SPo2 - 98%@RA
SYSTEMIC/ EXAMINATION -
CVS -S1,S2 Heard
RS-BAE+
CNS-NAD
P/A-Mild Splenomegaly+
Bowel sounds present
A
DIAGNOSIS-
DRUG INDUCED HEPATITIS
?BORDERLINE LEPROMATOUS LEPROSY
P-
1.IVF NS @75ML /HR WITH 1 AMP OF OPTINEURON IV/OD
2.INJ VIT K 1 AMP IN 100ML NS/IV/OD
3.TAB.UDILIV 300 MG/PO/BD
4.TAB OMNICORTIL 20MG PO/OD O-×
TAB OMNICORTIL 5MG PO/OD X-O
5.TAB ANTOXID PO/OD 2PM
6.TAB HEPTAGON PO/OD 2PM
7.SYP.LACTULOSE 10ML/PO/TID
8.FUDIC CREAM L/A
2/05/22
SOAP NOTES AMC BED -2
S -Yellowish discoloration of sclera +
No fresh complaints
O- Patient is consious, co-herent, co-operative,
No icterus,odema,Q cyanosis, clubbing, lymphadenopathy.
VITALS :
Temperature - 99.4F
Pulse rate - 78BPM, REGULAR, NORMAL VOLUME
BP -@8AM-120/80MM OF HG
SPo2 - 98%@RA
SYSTEMIC/ EXAMINATION -
CVS -S1,S2 Heard
RS-BAE+
CNS-NAD
P/A-Mild Splenomegaly+
Bowel sounds present
A
DIAGNOSIS-
DRUG INDUCED HEPATITIS
?BORDERLINE LEPROMATOUS LEPROSY
P-
1.IVF NS @75ML /HR WITH 1 AMP OF OPTINEURON IV/OD
2.INJ VIT K 1 AMP IN 100ML NS/IV/OD
3.TAB.UDILIV 300 MG/PO/BD
4.TAB OMNICORTIL 20MG PO/OD O-×
TAB OMNICORTIL 5MG PO/OD O-O
5.TAB ANTOXID PO/OD 2PM
6.TAB HEPTAGON PO/OD 2PM
7.SYP.LACTULOSE 10ML/PO/TID
8.FUDIC CREAM L/A
SOAP NOTES AMC BED -2 3/05/22
S -yellowish discoloration of sclera +
No fresh complaints
O- Patient is consious, co-herent, co-operative,
No icterus,odema, cyanosis, clubbing, lymphadenopathy.
VITALS :
Temperature - 98.6F
Pulse rate - 82BPM, REGULAR, NORMAL VOLUME
BP -@8AM-120/80MM OF HG
SPo2 - 98%@RA
SYSTEMIC/ EXAMINATION -
CVS -S1,S2 Heard
RS-BAE+
CNS-NAD
P/A-Mild Splenomegaly+
Bowel sounds present
A
DIAGNOSIS-
DRUG INDUCED HEPATITIS
? HANSENS DISEASE
P-
1.IVF NS @75ML /HR WITH 1 AMP OF OPTINEURON IV/OD
2.INJ VIT K 1 AMP IN 100ML NS/IV/OD D5
3.TAB.UDILIV 300 MG/PO/BD
4.TAB ANTOXID PO/OD 2PM
5.TAB HEPTAGON PO/OD 2PM
6.SYP.LACTULOSE 10ML7/PO/TID
7.FUDIC CREAM L/A











Comments
Post a Comment